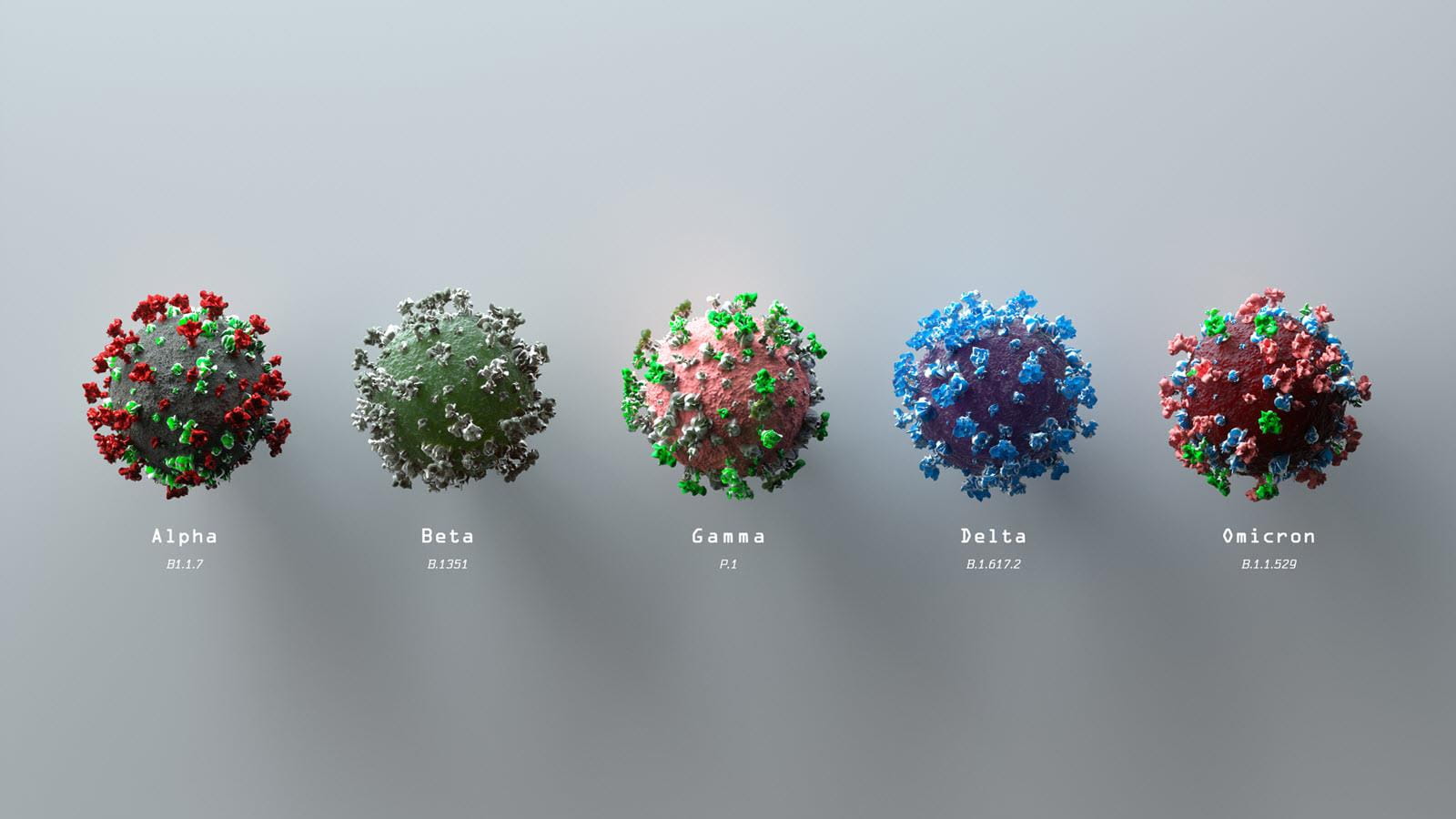
When U.S. health authorities authorized a second COVID-19 booster for Americans older than 50 last week they also endorsed a second booster for people who are moderately or severely immunocompromised, a group that includes organ transplant recipients and some who have primary immunodeficiencies.
For the immunocompromised, the recommendation had been four shots – a series of three primary doses of an mRNA vaccine followed by a booster. This latest recommendation for a second mRNA booster means an immunocompromised person could receive as many as five shots, including both the primary series and boosters.
Patients should ask their doctor whether a second booster is right for them. According to the new guidelines, the second booster should be given at least four months after the last one. During the recent Omicron surge, those who were boosted were 21 times less likely to die from COVID-19 compared to those who were unvaccinated and 7 times less likely to be hospitalized, according to the U.S. Centers for Disease Control.
“If you are moderately or severely immunocompromised (have a weakened immune system), you are at increased risk of severe COVID-19 illness and death,” the CDC says on its website. “Additionally, your immune response to COVID-19 vaccination may not be as strong as in people who are not immunocompromised.”
A U.S. Food and Drug Administration official added that research shows the vaccine’s ability to prevent serious symptoms decreases over time.
“Based on an analysis of emerging data, a second booster dose of either the Pfizer-BioNTech or Moderna COVID-19 vaccine could help increase protection levels for these higher-risk individuals,” said Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research.
The CDC says moderately to severely immunocompromised people include transplant patients, cancer patients and those who have moderate or severe primary immunodeficiency, such as DiGeorge syndrome and Wiskott-Aldrich syndrome.
Through the Immune Deficiency Foundation (IDF), immunologist Kate Sullivan, of the Children’s Hospital of Philadelphia, has been giving regular updates to PI patients throughout the pandemic. In a February update, she told patients that there is no defined definition of “moderate to severe” and that if patients wanted a booster – which was at that time was the fourth dose – they should get it.
With only a small number of exceptions, PI patients, even most of those with antibody deficiencies, have responded well to the mRNA vaccines, Sullivan said in her February 3 webinar for the IDF. Research shows patients produced an immune response similar to the general population, she said, thanks to mRNA vaccines, which are more powerful than traditional vaccines. One exception has been men and boys with X-Linked Agammaglobulinemia (XLA), Sullivan said.
Even people who don’t make antibodies to a tetanus vaccine, for instance, do make antibodies to SARS-CoV-2, the virus that causes COVID-19 when they get a course of mRNA vaccines, Sullivan said.
“People who don’t make antibodies to anything else, make antibodies to the SARS-CoV-2 virus,” she said.